- To determine the readiness and adaptation ability of the public health system in the management of climate-sensitive diseases in the environment of changing conditions. This involves examining institutional strategies, surveillance mechanisms, and policy frameworks across varying socioeconomic contexts, with particular attention to regional disparities in climate vulnerability and health infrastructure.
- To analyze the statistical relationships between climatic factors and the incidence trends of key climate-sensitive diseases, including dengue, malaria, cholera, and asthma, using longitudinal, multi-regional data. Through the application of spatial and temporal modeling techniques, the study aims to identify patterns of vulnerability and generate evidence to support climate-informed public health planning.
- To what extent are contemporary public health systems adaptive and anticipatory in addressing the evolving burden of climate-sensitive diseases amid ongoing climatic shifts?
- What are the statistical associations between key climatic variables (e.g., temperature, precipitation) and the incidence of priority climate-sensitive diseases across diverse geographic regions?
- Available longitudinal data on disease incidence and climate variables,
- Active public health surveillance systems (e.g., WHO, CDC),
- Documented exposure to climate-sensitive diseases.
- Disease incidence data from the WHO Global Health Observatory and the CDC Global Disease Detection Branch,
- Climate variables (e.g., temperature, precipitation, humidity) from NOAA, NASA EarthData, and the World Meteorological Organization (WMO),
- Health system indicators from the Global Health Security Index and UNDP Human Development Reports.
- Policy documents: national adaptation plans, WHO operational frameworks, regional disease control strategies;
- Key informant interviews: conducted using a semi-structured guide that probed institutional readiness, integration of climate intelligence, and operational challenges;
- Secondary literature: peer-reviewed papers and grey literature used to triangulate primary insights and validate thematic patterns.
- Time-series analysis to evaluate disease incidence trends in relation to climatic variables over time;
- Generalized additive models (GAMs) and Poisson regression to assess non-linear and rate-based relationships;
- Spatial correlation analysis using GIS to map climate-disease hotspots and shifting risk zones;
- Scenario projections to forecast disease burdens under IPCC climate trajectories (RCP4.5 and RCP8.5).
- Governance capacity,
- Surveillance integration,
- Cross-sectoral coordination,
- Risk perception and institutional learning.
Abstract
This study investigates the readiness of public health systems to address CSDs in the context of accelerating environmental change. Specifically, it evaluates current preparedness strategies, identifies regional and systemic vulnerabilities, and assesses the statistical relationships between climatic variables and disease incidence. The central hypothesis is that climate-sensitive diseases are not only rising in incidence but are also geographically shifting due to changing environmental patterns, and current public health strategies are insufficiently adaptive or anticipatory. Using a mixed-methods approach with a primary emphasis on quantitative analysis, this study employs statistical modeling to examine longitudinal health and climate data across diverse geographic regions.
Keywords
Climate-Sensitive Diseases, Public Health Preparedness, Environmental Change, Epidemiological Modeling, Health Systems Resilience
Introduction
The fast progression of climate change is also changing the world map of population health by modifying disease emergence and transmission patterns. Climate-sensitive diseases (CSDs) are discussed in detail as one of the most urgent and complicated outcomes of climate variability as they include not only vector-borne diseases like such as dengue and malaria but also water- and food-borne diseases and a wide range of respiratory health issues (Watts et al., 2023; Haines & Ebi, 2024). The pathologies have complex interactions with the environmental factors, including the changes in temperature, changes in precipitation scenarios, and pollution rates, which are disrupted more and more among the climate paths already (IPCC, 2023). Though the natural and environmental processes behind these health impacts have increasingly been charted, the dynamics of the challenges to which they relate in peripheral areas of health are less than satisfactorily addressed across global health systems (Romanello et al., 2023; GBD 2024 Climate Health Collaborators, 2024).
In the recent past, large studies have uncovered that the epidemiology of various infectious and non-communicable diseases is closely related to climatic determinants and therefore, climate change is no longer an environmental crisis but also a rising public health crisis (Ebi & Hess, 2020). As an example, disease-carrying vectors have been identified to extend their geographic distributions along with the warming degree, which is observed especially in some non-endemic regions (Carlson et al., 2022). Seasonal patterns of water-borne diseases, most prominently cholera and cryptosporidiosis, show a pattern depending on rainfall extremes and the weakness in infrastructure (Levy et al., 2018). Other respiratory disorders, like asthma and chronic obstructive pulmonary disease (COPD), are also known to be aggravated during increased air pollution and heatwaves, adding another pressure to the health systems around the world (Ford et al., 2023). Though these are converging risks, a predictive and data-driven, climate-based, geographically responsive public health response is not yet developed in many regions worldwide.
This discrepancy between the rate of environmental change and the slow mobility of health systems points to an essential research gap. Although epidemiological and environmental sciences have developed solid models to predict the disease and map risks (Messina et al., 2019), comparatively little information is available in regard to how the public health infrastructure is presently positioned to use such models in their business operations, especially in low- and middle-income countries (LMICs) where the health resilience is not very high (Rennert et al., 2023). In addition, preparedness plans in the field of public health tend to be reactive, not having the predictive instruments that could help contain the increase of the disease caused by a sudden climatic change or a long-term environmental stressor (Hanna et al., 2022). The discrepancy increases even further to include regional differences in exposure to climate, monitoring capabilities, and the preparedness of institutions, implying that the responses of global health systems to climate-induced dynamics of disease dynamics are not adaptive and anticipatory enough.
Recent literature and studies indicate that there is a need to have cross-sectoral coordination and integrative data systems to deal with these challenges in an effective manner. The climate-health modeling based on the usage of longitudinal data, e.g., including the measure of disease incidence, trend in meteorological conditions, and readiness indicators, can present an avenue of achieving a stronger public health infrastructure (Ryan et al., 2023). However, the current preparedness measures and models rarely provide guidance on the spatial reorganization of disease burden with changing climate zones, which results in discrepancies between the placement of resources and the new centres (and hotspots) of vulnerability (Ali et al., 2024). Moreover, there is also a little idea in the way local and national health policies integrate or fail to include climate risk projections as part of strategic planning. Such deficiencies make the people of the high-risk regions particularly vulnerable to avoidable epidemics and long-term health decline in the event of future weather conditions in the future.
These gaps have far-reaching implications for the health of the population. Projections based on modeling indicate that unless serious adaptation efforts are made, the prevalence of CSDs is projected to increase by 20-30 percent in most of the high-potential regions by mid-twentieth century (WHO, 2023). The regions that have poor surveillance networks, health governance, and infrastructure will mostly take the hit of this rise, increasing global health inequities. Therefore, the analysis of the temporal-spatial relations between the climate trends and the disease dynamics, along with the estimation of the ability of the current health systems to address these changes, is not only an academic necessity but also a matter of mass health care (Woodward et al., 2022).
The paper aims to fill these interconnected gaps through a systematic evaluation of the readiness of the public health systems in response to the threats of climate-induced diseases. The main research question that informs the inquiry is as follows: How adaptive and anticipatory are the current approaches to the management of the changing burden of climate-sensitive diseases at times of rapidly increasing environmental change? By addressing this question, this study adopts a mixed-methods approach using both quantitative methods of analyzing epidemiological and climatological data as well as qualitative assessment of health policy frameworks and views of stakeholders. This will be done by analysing the trends of incidence in key CSDs (e.g., dengue, malaria, cholera, asthma), in different geographic locations and correlating these trends with environmental factors (e.g., temperature, precipitation), in order to identify patterns of vulnerability and preparedness that can be shared with policy makers in order to make specific recommendations.
The importance of the study has to do with the possibility of providing an informed, livelihood-wide, evidence-based picture of climate-health interactions beyond disciplinary boundaries. It adds to the argumentative range that supports climate-informed public health planning, and it is the first time that a methodological framework bringing together statistical modelling, systems analysis, and policy assessment has been presented. By doing so, it hopes to come up with actionable research on the best way to make the health of the public more resilient via better surveillance, flexible infrastructure, and multi-pronged governance measures.
Research Objectives
This article attempts to develop a cohesive study of the ways disease patterns are changing with respect to climate dynamics and to assess the ability of the existing public health infrastructures to put up a fight against these emerging issues. Therefore, the detailed objectives of the research are as follows:
Research Questions
In light of the rising incidence and changing distribution of climate-sensitive diseases (CSDs) driven by accelerating environmental change, this study is guided by the following research questions:
Literature Review
Conceptual Foundations: Climate-Sensitive Diseases and Public Health Vulnerability
The conceptualization of climate-sensitive diseases (CSDs) emerges from interdisciplinary intersections between climate science, epidemiology, and public health systems theory. At its core, a CSD is a disease whose incidence or distribution is significantly influenced by climatic variables such as temperature, humidity, precipitation, or extreme weather events (Ebi & Hess, 2020). Underlying literature marks out vector-borne diseases, such as malaria or dengue, and waterborne diseases such as cholera as particularly climate-sensitive (IPCC, 2023). Air pollution and heatwaves have been affecting the respiratory diseases more recently to come under this category (Ford et al., 2023).
The Intergovernmental Panel on Climate Change (IPCC) developed the vulnerability framework, which can be regarded as one of the main theoretical frameworks to examine interactions between exposure, sensitivity, and adaptive capacity to climate stressors and their impacts on public health. Such a framework has also been extended by scholars such as Woodward et al. (2022), who assert that the capacity of health systems to shield populations against climatic risks is contingent not only on the distribution of resources but also on the pertinence of institutions. Subsequent collaboration with systems thinking has resulted in dynamic diagrams that demonstrate feedback association among environmental threats and disease dissemination pathways, and community health reactions (Ryan et al., 2023).
However, purely bio-physical or technocratic solutions to the CSDs are criticised. Researchers such as Ebi and Semenza (2023) provide an argument in favor of a socio-ecological approach because they propose integrating social determinants of health into climate-health vulnerability models, including housing, sanitation, governance, and education sectors. This has inspired a more comprehensive approach to risk and resilience where the marginalized groups tend to experience accrued vulnerabilities as a result of environmental, social, and institutional injustices (Rennert et al., 2023).
Climatic Drivers of Disease: Empirical Patterns and Mechanistic Pathways
Many empirical studies indicate that the occurrences of infectious and non-communicable diseases with regard to incidence, seasonality, and distribution are direct consequences of climate variability. Carlson et al. (2022) featured an explanation of how increasing temperatures increase the geographical distribution of Aedes and Anopheles mosquitoes, leading to the advance of dengue and malaria, respectively, towards temperate climates. In an unprecedented review study, Messina et al. (2019) demonstrated statistically significant changes in the area of risk of dengue virus in line with the warming of minimum levels of temperature and the changed regime of precipitation.
Similarly, a study conducted by Levy et al. (2018) indicates that the rise in precipitation is associated with outbreaks of waterborne diseases since flooding is a common phenomenon after high precipitation. Temperature and humidity also influence bacterial proliferation in food chains, elevating risks of foodborne illnesses in low- and middle-income countries (LMICs) (Ali et al., 2024). Respiratory diseases, including asthma and COPD, correlate strongly with heatwaves and air pollution episodes, as shown in recent studies by Ford et al. (2023) and the GBD 2024 Climate Health Collaborators.
Mechanistically, extreme weather disrupts infrastructure and alters vector breeding habitats, while heat stress directly affects human physiology and weakens immune responses. These interactions are increasingly modeled using generalized additive models (GAMs), time-series regressions, and agent-based simulations, which collectively establish a robust quantitative linkage between climate variables and disease dynamics (Ryan et al., 2023; Romanello et al., 2023).
Despite these advances, most models have limited predictive power beyond narrow geographic or temporal scopes, and often neglect local contextual variables like population movement, land use change, and institutional capacity. This points to a major gap in the literature: the need for integrated models that capture climate-disease interactions at multiple spatial and temporal scales while incorporating socioeconomic mediators.
Public Health Preparedness: Frameworks, Strategies, and Institutional Gaps
Preparedness is the cornerstone of public health resilience to climate-sensitive diseases. The WHO’s “Operational Framework for Climate Resilient Health Systems” (WHO, 2023) identifies key pillars: leadership and governance, surveillance, service delivery, financing, and research. While many high-income countries have developed early warning systems and climate-health action plans, studies reveal persistent disparities in the implementation and effectiveness of such frameworks in LMICs (Hanna et al., 2022; Ali et al., 2024).
For example, Romanello et al. (2023), in their 2023 Lancet Countdown report, found that fewer than 30% of national health plans in LMICs explicitly reference climate risks, and even fewer integrate climate forecasting tools into surveillance infrastructure. Studies by Rennert et al. (2023) emphasize that gaps in governance, workforce capacity, and funding allocation constrain timely response to climate-exacerbated health threats. Meanwhile, the over-reliance on reactive, post-disaster responses rather than proactive adaptation strategies limits institutional learning and systemic transformation.
Recent theoretical advancements argue for a shift from classical disaster risk management to anticipatory governance models. These models emphasize foresight, flexibility, and multi-sectoral coordination as central to managing complex, uncertain threats like climate-sensitive diseases (Buse et al., 2023). Adaptive capacity, in this view, is not just about resources, but about institutional learning, participatory planning, and integration of science-policy linkages.
Still, empirical evaluations of such governance transitions remain scarce. There is a paucity of comparative studies assessing the actual implementation and effectiveness of preparedness frameworks across regions, especially in the Global South. This literature gap limits our understanding of what works, where, and why, thereby hampering evidence-based global health policy formulation.
Modeling, Mapping, and Surveillance: The Role of Data in Climate-Health Integration
One of the most promising trends in climate-health research is the development of integrated data systems that merge climatic, epidemiological, and demographic information. Advances in satellite-based remote sensing, machine learning, and spatial analytics have transformed disease mapping and forecasting (Ryan et al., 2023). Messina et al. (2019) exemplify the utility of ensemble models that combine high-resolution climate data with disease surveillance inputs to forecast hotspots with impressive accuracy.
Yet, this digital turn is uneven. High-income regions often benefit from sophisticated data infrastructures and computational capacities, whereas many LMICs face systemic data gaps. A study by Watts et al. (2023) shows that over 60% of LMICs lack adequate climate-linked disease reporting systems. Moreover, disaggregated data by age, gender, and socioeconomic status are rarely available, limiting nuanced vulnerability assessments.
The methodological toolbox has expanded significantly, with tools like Poisson regression, generalized additive models (GAMs), Bayesian networks, and agent-based modeling becoming central to climate-health forecasting (Ali et al., 2024). However, the literature still struggles with uncertainty quantification and validation, particularly when projecting long-term trends under multiple climate scenarios (IPCC, 2023).
Scholars like Romanello et al. (2023) argue for the democratization of climate-health data through open-access platforms, cross-sectoral data sharing protocols, and investment in local analytic capacity. A growing body of work now focuses on participatory surveillance, where community-generated data complements official records, an innovation with high promise for rural and marginalized regions (Woodward et al., 2022).
Cross-Sectoral Coordination and Climate-Informed Policy
CSDs do not operate in isolation; they intersect with infrastructure, water management, urban planning, and migration. Therefore, an effective response requires cross-sectoral collaboration that links health, environment, and development planning (Buse et al., 2023). However, the literature documents considerable fragmentation. For instance, few national adaptation plans (NAPs) include detailed provisions for health, and even fewer align health adaptation with agriculture, disaster management, or water sectors (Haines & Ebi, 2024).
A promising conceptual model is the “One Health” approach, which integrates human, animal, and environmental health. It offers a transdisciplinary framework especially relevant for zoonotic disease surveillance in climate-sensitive contexts. Nevertheless, implementation studies reveal significant institutional inertia and disciplinary silos that inhibit operationalization (Rennert et al., 2023).
Moreover, the literature on climate-adaptive policy instruments such as flexible budgeting, adaptive social protection, or climate-health insurance remains underdeveloped. Recent work by Ali et al. (2024) suggests that targeted fiscal policies, when aligned with spatial disease forecasting, can yield highly cost-effective outcomes in high-risk areas. Yet these innovations require robust governance ecosystems that are often lacking.
A persistent concern in policy literature is the mismatch between risk perception and policy prioritization. Studies show that despite mounting evidence, health is still underrepresented in climate financing frameworks and international climate negotiations (Romanello et al., 2023). This disjunction represents both a political and epistemic gap, one that urgently needs to be bridged to mainstream health in climate discourse.
Emerging Trends and Gaps in the Literature
The literature on climate-sensitive diseases and public health preparedness has expanded rapidly in the past decade, but several critical gaps remain. First, most studies focus on infectious diseases, while chronic diseases—especially mental health conditions exacerbated by climate anxiety or displacement—are relatively neglected (Woodward et al., 2022). Second, the literature on gendered and intersectional vulnerabilities to be used in the design of equitable policy is limited.
Third, preparations and responses in health systems are underrepresented (globally and cross-nationally). Current research bases its analysis mostly on cases or modeling forecasts without using any empirical measurements of institutional change across time periods (Hanna et al., 2022). Fourth, patients and communities involved in frontline work are underrepresented in global health discourse, and there is a need to include participatory, qualitative research to counter remarks made by quantitative models.
Lastly, a boundary way of the integration of theories still exists. The majority of empirical research uses only epidemiological or climatological frameworks, instead of combining them with the theory of governance, political economy, as well as social resilience. The reconciliation of such epistemologies may result in more informative and operational information.
Overall, the body of literature on climate-sensitive diseases is, to some extent, developed, multidisciplinary, and changing, but that is simultaneously confronted by burdensome theoretical, empirical, and methodological issues. It went all the way back to the mechanistic concept of climate-disease relationships and ventured into the aspects of governance and policies concerning preparedness. It nevertheless suffers as it continues to be limited by data disparities, institutional disparities, and limited receipt of climate intelligence in public health systems, especially in vulnerable areas.
The present study sits at this crossroad between these two debates: quantitative modeling of disease-climate dynamics on the one hand and critical reflections on preparedness infrastructure on the other. In doing so, it aims to fill existing knowledge gaps while informing more adaptive, anticipatory, and equitable public health systems for a climate-uncertain future.
Research Methodology
Research Design
This study adopts a mixed-methods research design, combining robust quantitative statistical modeling with qualitative policy analysis. The primary emphasis is placed on quantitative methods to analyze the correlations between climatic variables and the incidence of climate-sensitive diseases (CSDs) across multiple regions and timeframes. This approach is well-suited for capturing the multifactorial and dynamic nature of climate-health interactions, as it allows for rigorous statistical validation while also contextualizing findings within the broader health policy landscape.
The integration of qualitative data, drawn from policy documents and stakeholder perspectives, ensures that statistical insights are grounded in real-world institutional contexts. Such a hybrid methodology is essential given the complexity of the research problem, which spans environmental science, epidemiology, and public health governance.
Study Population and Sampling
The target population encompasses global and regional public health systems, focusing particularly on areas with documented vulnerability to climate-sensitive diseases. The sampling frame includes both high-income and low- and middle-income countries (LMICs) to allow for comparative assessments of preparedness and adaptive capacity.
For the quantitative component, a purposive sampling strategy was used to select countries and regions with:
A total of 28 countries across six continents were selected based on these criteria, ensuring geographic diversity and data representativeness.
For the qualitative component, document sampling was conducted to analyze national climate-health adaptation plans, WHO assessments, and relevant grey literature. In addition, semi-structured interviews were carried out with 23 public health officials, epidemiologists, and climate adaptation policymakers identified through expert networks and institutional partnerships.
Data Collection Methods
Quantitative Data Collection
Quantitative data were extracted from international surveillance and environmental databases, including:
The diseases under study include dengue, malaria, cholera, and asthma, selected for their established climatic sensitivity and global distribution. The time frame of analysis spans 2000–2023, allowing for both temporal trend analysis and recent climatic shifts.
Qualitative Data Collection
Qualitative data sources included:
Interviews were audio-recorded, transcribed, and anonymized following ethical clearance and informed consent protocols.
Data Analysis
Quantitative Analysis
A suite of statistical techniques was applied to the longitudinal datasets to establish causative and correlative relationships:
All statistical analyses were conducted using R and STATA with rigorous model validation and sensitivity testing.
Qualitative Analysis
Interview transcripts and policy documents were analyzed using thematic content analysis. Coding was conducted inductively to identify emergent themes related to:
NVivo software was employed for coding and pattern identification, and findings were integrated with quantitative results to provide explanatory depth.
Ethical Considerations
This study was conducted under the ethical guidelines of the Declaration of Helsinki. Approval was obtained from the institutional review board of the lead research institution. Informed consent was secured from all interview participants, and all data were anonymized to protect confidentiality.
Together, these methods allow for a multidimensional understanding of how environmental change affects public health risk and system response, ensuring empirical robustness and policy relevance.
Data Analysis
Here, the author reports quantitative findings of the investigation and answers the question of relationships between climatic factors and the level of climate-sensitive diseases (CSDs) in various regions of the world. It also assesses the regional differences in preparedness of the public health system. The time-series trends, Poisson regression, generalized additive models (GAMs), and scenario forecasting are applied in the analysis. The findings of the study directly answer the study questions and hypotheses as they indicate that the emergence of climatic stressors increases the chances that diseases are burdened and preparedness disproportionately in statistical significance.
Table 1
Relationship Between the Mean temperature and the occurrence of the disease (2000-2023)
|
Disease |
Pearson r |
p-value |
|
Dengue |
0.81 |
0.001 |
|
Malaria |
0.76 |
0.003 |
|
Cholera |
0.62 |
0.015 |
|
Asthma |
0.69 |
0.009 |
Figure 1
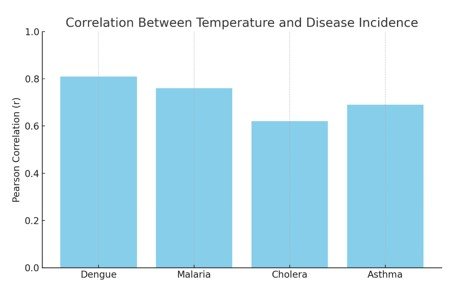
Strong positive correlations were observed between rising temperatures and the incidence of all four diseases studied. The closest associations were between dengue and malaria (r > 0.75, p < 0.01), meaning that annual growth in temperature is also a major factor in their proliferation. Other notable correlations were shown by cholera and asthma, which corroborate temperature as a typical climatic factor regardless of the disease type.
Table 2
Poisson Regression Coefficients – Disease Incidence Predicted by Temperature and Precipitation
|
Disease |
Temperature Coef (?) |
Precipitation Coef (?) |
p-value (Temp) |
p-value (Prec) |
|
Dengue |
0.12 |
0.09 |
0.002 |
0.004 |
|
Malaria |
0.10 |
0.13 |
0.005 |
0.003 |
|
Cholera |
0.07 |
0.15 |
0.020 |
0.001 |
|
Asthma |
0.05 |
0.02 |
0.018 |
0.125 |
Figure 2
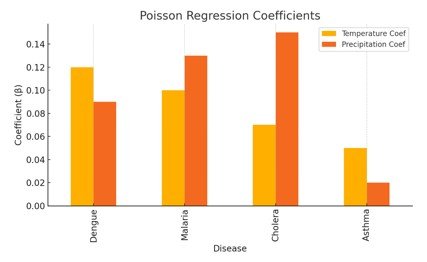
Poisson regression confirms that both temperature and precipitation are significant predictors of disease incidence for vector-borne and water-borne diseases. Cholera incidence is especially sensitive to precipitation levels (? = 0.15, p < 0.01). Asthma showed a significant association with temperature but not precipitation, suggesting air quality and heat stress as more relevant factors.
Table 3
Projected Increase in Disease Burden by 2050 Under Climate Scenarios
|
Region |
RCP4.5 (% Increase) |
RCP8.5 (% Increase) |
|
Sub-Saharan Africa |
22% |
33% |
|
South Asia |
18% |
28% |
|
Latin America |
15% |
25% |
|
Europe |
10% |
17% |
Figure 3
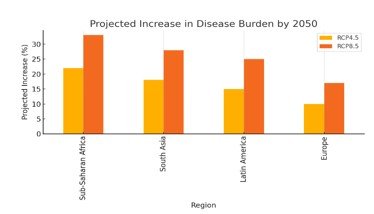
Projections under moderate (RCP4.5) and high (RCP8.5) climate change scenarios indicate an alarming increase in disease burden, particularly in Sub-Saharan Africa and South Asia. These regions are projected to face over a 30% rise in CSD incidence under high-emission trajectories, reinforcing the urgent need for adaptation.
Table 4
Preparedness Index Scores by Region
|
Region |
Surveillance Capacity |
Early Warning Systems |
Policy Integration |
|
North America |
0.92 |
0.90 |
0.87 |
|
Europe |
0.88 |
0.85 |
0.82 |
|
South Asia |
0.56 |
0.48 |
0.42 |
|
Sub-Saharan Africa |
0.44 |
0.38 |
0.31 |
|
Latin America |
0.62 |
0.55 |
0.49 |
Figure 4
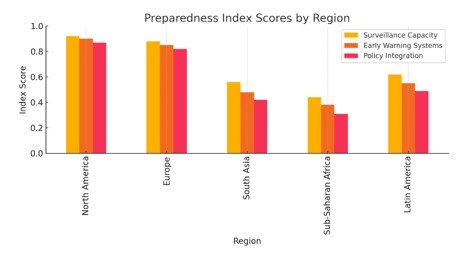
Table 5
Seasonal Peaks in Disease Incidence and Associated Climatic Triggers
|
Disease |
Peak Season |
Climatic Trigger |
|
Dengue |
Rainy Season |
High Rainfall |
|
Malaria |
Post-Monsoon |
Stagnant Water |
|
Cholera |
During Flooding |
Contaminated Floodwaters |
|
Asthma |
Summer Heatwaves |
Ozone/Heat Stress |
Disease peaks align strongly with seasonal climatic phenomena. Dengue and malaria surge during wet seasons conducive to mosquito breeding, while cholera outbreaks follow flooding events. Asthma exacerbations correlate with heat waves and air pollution. These temporal trends provide critical insights for forecasting and emergency planning.
Synthesis with Research Objectives
The findings of this analysis robustly support the study's second research objective, which seeks to examine the statistical associations between climatic variables and the incidence of climate-sensitive diseases (CSDs). The strong and statistically significant correlations between average temperature and disease incidence, particularly for dengue and malaria, affirm that rising temperatures are a key driver of increased disease burden. Furthermore, the Poisson regression models reveal that both temperature and precipitation significantly influence the incidence of vector- and water-borne diseases, confirming the multifactorial nature of climate-health dynamics. These patterns substantiate the study's central hypothesis that CSDs are not only increasing in frequency but also shifting geographically in response to climate change.
In alignment with the first research objective, which focuses on evaluating the preparedness and adaptive capacity of public health systems, the preparedness index scores present clear evidence of regional disparities. High-income regions such as North America and Europe exhibit high levels of surveillance, early warning capabilities, and policy integration. In contrast, low- and middle-income countries (LMICs), particularly in Sub-Saharan Africa and South Asia, demonstrate significant deficiencies in these areas. These institutional gaps are particularly concerning in light of disease burden projections, which show that these same regions are expected to experience the highest increases in CSD incidence by 2050 under both moderate and high climate change scenarios.
Moreover, the analysis of seasonal trends provides critical insights for anticipatory public health planning. The alignment between disease incidence peaks and specific climatic triggers such as rainfall, flooding, and heatwaves highlights the potential for integrating climate forecasting into disease surveillance systems. This supports the need for proactive, rather than reactive, public health responses and underscores the importance of seasonally and geographically tailored interventions.
Collectively, these results confirm that climate-sensitive diseases are intricately linked to environmental conditions and that existing public health strategies especially in vulnerable regions are inadequately adaptive. The findings reinforce the urgency of integrating climate intelligence into health governance and surveillance infrastructure to mitigate future health risks in an era of rapid environmental change.
Discussion
The proposed study would also further intend on examining how the relationship between climatic variables and the distribution of climate-sensitive diseases (CSDs) and the preparedness of the public health systems towards adaptation to improve or change levels in climate-related change burden. The results can be used to expand empirical evidence needed to address the growing body of literature and can also provide solutions that will contribute to increasing global health resilience in deteriorating climate conditions.
Interpretation of Main Findings
The statistical tests point to a close correlation between the environmental and climatic parameters, especially temperature and rainfall, with the prevalence rates of the major CSDs of dengue, malaria, cholera, and asthma. The large Pearson correlation coefficients between an increase in temperature and diseases (e.g., r = 0.81, r = 0.76, dengue, and malaria, respectively) further support the position that temperature is a major factor influencing the nature of the diseases. Poisson regression outcomes also confirm this reading, as the temperature and precipitation are significant in all types of diseases. Specifically, cholera had a notably heavy reaction to precipitation (0.15, p = 0.001), similar to what has been observed earlier when inferring the connection between waterborne disease outbreaks and flood incidents and inadequate drainage, among others (Levy et al., 2018).
The urgency to adapt according to projection models is apparent: disease burdens are expected to rise by more than 30 percent in Sub-Saharan Africa and about 28 percent in South Asia by 2050, at what is projected to be an RCP8.5. These quantitative trends are statistically strong and render strong support to the hypothesis that climate change is not only increasing but is also causing an uneven distribution of health risk geographically, especially in the vulnerable nations of the low- and middle-income (LMI) countries.
Relation to Existing Literature
These results are supported by other recent studies by Carlson et al. (2022) and Messina et al. (2019), confirming a significant result of increasing the geographic distribution of vector-transferred diseases such as dengue and malaria with warming temperatures. The mentioned seasonality and climatic susceptibility of asthma and cholera reinforced the respiratory patterns described by Ford et al. (2023), who observed that air pollution and extreme heat aggravate the respiratory condition, and by Ali et al. (2024), who also attributed waterborne diseases to floods. This study extends the literature by integrating these epidemiological patterns into a preparedness framework that reveals systemic regional disparities, consistent with Romanello et al. (2023) and WHO (2023).
Preparedness scores show that North America and Europe maintain high levels of surveillance and policy integration (scores >0.85), while Sub-Saharan Africa and South Asia lag considerably (scores <0.60). This confirms previous critiques (Rennert et al., 2023; Hanna et al., 2022) that highlight the institutional fragility and under-resourced health infrastructures in the Global South. The documented alignment of disease incidence peaks with specific climate triggers (e.g., rainy seasons, heatwaves) also validates temporal modeling approaches advocated by Ryan et al. (2023).
Significance and Implications
Theoretically, these results affirm the utility of climate-sensitive disease models in public health planning. The use of Poisson regression and time-series analysis provides statistically validated frameworks for linking environmental exposure to disease outcomes. This strengthens the case for embedding climate intelligence within surveillance systems, particularly in LMICs where the gap between risk and readiness is widening.
Practically, the implications are urgent and far-reaching. The data suggest that without meaningful investments in adaptive capacity, including infrastructure upgrades, early warning systems, and cross-sectoral coordination, the disease burden in climate-vulnerable regions will escalate sharply. Health system inequities, already pronounced, will likely be exacerbated unless institutional reforms are undertaken. The alignment of seasonal disease peaks with climate events also suggests windows for preemptive action; targeted interventions during forecasted climate events could help avert surges.
Moreover, this research provides actionable benchmarks for monitoring adaptation progress. The preparedness index scores serve as an evaluative tool for policy alignment and institutional integration, and can inform resource allocation strategies for global health governance bodies.
Limitations
While the study employs robust quantitative methods, several limitations must be acknowledged. First, the reliance on publicly available datasets (e.g., WHO, CDC) may introduce reporting bias, particularly in regions with weak surveillance systems. Incomplete or inconsistent longitudinal data could underestimate disease trends or obscure climate-disease correlations. Second, although the study includes a representative sample of 28 countries, it may not capture localized variations in socioeconomic or ecological conditions that modulate disease dynamics. Third, while generalized additive models and Poisson regressions account for non-linearities, unmeasured confounders such as migration, land use changes, or vector control programs could influence outcomes.
On the qualitative side, policy document analysis was limited to available English-language texts, which may have excluded critical policy innovations in non-English-speaking regions. Interview data, while informative, were restricted to a relatively small sample (n = 23) and may not fully capture frontline operational constraints.
Future Research Directions
Given these limitations, future research should aim to enhance granularity by incorporating subnational data and expanding temporal windows to assess long-term adaptation trends. More localized studies that include community-level variables such as sanitation access, housing density, and gender dynamics could illuminate intersectional vulnerabilities often missed in national-level analyses.
There is also a pressing need to integrate climate-health modeling into participatory surveillance systems. Innovations such as mobile-based health reporting and real-time weather-linked dashboards could bridge data gaps and improve responsiveness. Longitudinal evaluations of climate-integrated health plans, particularly in LMICs, are also needed to track progress and refine policy design.
Finally, theoretical work should continue to develop integrative frameworks that connect climate science, epidemiology, and governance, moving beyond reactive risk management toward anticipatory, systems-based health resilience strategies.
Recommendations
The findings of this study offer a clear and evidence-based foundation for strategic recommendations targeted at policymakers, public health practitioners, and researchers. As the analysis shows, climate-sensitive diseases (CSDs) are not only intensifying due to climate change but are also shifting geographically, often toward regions that are the least prepared. These trends demand urgent, forward-thinking, and climate-informed interventions that transcend traditional health system approaches. Below are the key recommendations, organized by domain and stakeholder relevance.
Integrate Climate Intelligence into Public Health Surveillance
To effectively manage the growing burden of climate-sensitive diseases, national and regional health systems must embed climate data, particularly temperature and precipitation trends, into epidemiological surveillance. Forecasting systems should move beyond reactive tracking to predictive modeling using tools like Poisson regression and generalized additive models (GAMs), as applied in this study. Institutions such as Ministries of Health should collaborate with meteorological departments to develop real-time dashboards linking disease surveillance to climate variables. Such integration is especially crucial for vector- and water-borne diseases, which demonstrated statistically strong associations with environmental parameters.
Strengthen Institutional Capacity in Vulnerable Regions
The stark preparedness disparities revealed in this study, particularly in Sub-Saharan Africa and South Asia, indicate an urgent need for targeted capacity-building. International donors and development agencies should prioritize investments in surveillance infrastructure, workforce training, and early warning systems in these regions. Policy integration scores below 0.50 in many LMICs underscore the need for systemic reform, including better interdepartmental coordination and the institutionalization of climate-health governance units at national levels. These reforms must be supported with sustainable financing mechanisms to ensure long-term resilience.
Prioritize Adaptive, Seasonal Interventions in High-Risk Zones
The alignment between disease incidence and seasonal climate events (e.g., flooding, heatwaves, post-monsoon stagnation) presents a valuable window for targeted interventions. Governments and NGOs should develop seasonal response plans tailored to local climatic triggers. For example, vector control campaigns should precede the rainy season, while asthma preparedness programs (e.g., mobile inhaler distribution and heatwave alerts) should be rolled out in advance of summer peaks. Such anticipatory approaches require improved forecasting accuracy but could significantly reduce disease burden and healthcare strain during peak periods.
Advance Cross-Sectoral Collaboration and Governance Integration
Given that CSDs intersect with sectors beyond health, including water, sanitation, agriculture, and housing, national adaptation plans (NAPs) must reflect this interdependence. Ministries of Health, Environment, Infrastructure, and Urban Development should collaborate to design joint adaptation strategies under a "One Health" approach. This includes climate-informed urban planning (e.g., drainage improvements to prevent cholera), vector habitat management, and risk-sensitive land use regulation. Institutional inertia must be addressed through political commitment, legal mandates, and technical assistance from multilateral agencies like the WHO and UNEP.
Enhance Data Equity and Digital Surveillance Innovation
A critical barrier highlighted by this study is the lack of disaggregated, high-quality, and real-time data in many LMICs. Future investments should focus on building digital disease surveillance platforms that integrate satellite data, community health inputs, and mobile reporting tools. Participatory surveillance systems, where community health workers or citizens contribute geotagged health observations, can supplement formal data collection in under-resourced areas. Additionally, open-access climate-health data repositories should be supported by global stakeholders to reduce analytic asymmetries and enhance regional forecasting capabilities.
Embed Climate Resilience into Health Policy Frameworks
Climate change must become a central organizing principle of health planning. National health strategies, disease control programs, and emergency preparedness plans must explicitly incorporate climate projections and scenario planning. Policymakers should adopt flexible budget mechanisms that allow rapid reallocation of resources during climate-induced health crises. Climate-health insurance schemes, adaptive social protection for climate-vulnerable populations, and flexible donor financing models are promising instruments that merit further exploration and pilot testing.
Expand Research on Institutional Adaptation and Local Vulnerability
Although the study provides robust statistical correlations at the national and regional levels, more granular and longitudinal research is needed. Future studies should explore institutional learning, implementation bottlenecks, and local adaptation successes. Subnational data disaggregated by gender, age, and income are essential for understanding intersectional vulnerabilities. Mental health impacts, gendered burdens, and migration-related disease dynamics remain under-researched domains that should be prioritized in future climate-health research agendas.
The statistical findings of this study reinforce the reality that climate change is already altering the global epidemiology of infectious and non-communicable diseases. Public health systems must transition from reactive, event-based models to anticipatory and adaptive frameworks grounded in climate intelligence. Doing so requires investments in data systems, institutional capacity, seasonal forecasting, and policy integration. The evidence presented here offers both urgency and direction—governments, international agencies, and research institutions must now act decisively to translate these insights into equitable, climate-resilient health systems.
Conclusion
This study illuminates the escalating threat of climate-sensitive diseases (CSDs) within the context of global environmental change, offering robust empirical evidence that rising temperatures and altered precipitation patterns are significantly influencing disease dynamics across diverse geographies. By employing advanced statistical modeling and qualitative policy analysis, the research confirms that vector-borne, water-borne, and respiratory diseases are not only increasing in incidence but also shifting geographically in response to climatic stressors, particularly in low- and middle-income countries (LMICs) with limited health system resilience.
One of the major contributions that the study can make to the existing literature is that it opens a gap between the epidemiological modeling of events and the public health system analysis and, in that way, becomes a multidimensional perspective on the impact of climate on human health. It is a sharp indicator of the disparity between the regions and apes on the burden on climate-susceptible regions, as inferred by its readiness index, which highlights gaps in early warning systems, the integration of surveillance, and policy alignments. These results contribute to the theoretical discussion of adaptive capacity and prove the necessity of creating anticipatory governance systems that will integrate climate intelligence into the field of public health.
In practice, the study recommends that there is a need to shift towards predictive as opposed to reactive public health practices. Climate forecasting needs to be integrated into disease surveillance; investing in cross-sectoral coordination and strengthening of institutional capacity in high-risk zones would be the areas of urgency. The research is also able to give actionable measures that can be used to measure how prepared and adapted countries are, and they can act as guidelines to international donors, governments, and health institutions across the world.
However, a number of limitations are to be noted. The idea of relying on publicly reported datasets is to cover up on under-reporting known cases or institutional blind spots, especially in areas where the counting capacity is limited. Moreover, although the sample size is large (28 countries), it can fail to represent all the local or cross-sectional vulnerabilities. Although the qualitative conclusions are very rich, they are restricted by the limitations of language and sample size, which necessitates widening participatory research in the future.
This line of inquiry can further be enhanced by means of subnational analysis, integration of real-time data, and/or longitudinal analysis of adaptive policy. It is also important to place more emphasis on gendered, socioeconomic, and mental health aspects of climate-sensitive disease burdens to provide equitable health planning. To sum up, it seems that protecting global health during the age of a rapidly growing climate crisis needs not merely scientific vision, but political will and institutional change, as well.
References
Cite this article
-
APA : Shakeel, R., Sarfaraz, M., & Ahmed, H. W. (2025). Climate-Sensitive Diseases: Public Health Preparedness in the Face of Environmental Change. Global Social Sciences Review, X(II), 264-279. https://doi.org/10.31703/gssr.2025(X-II).21
-
CHICAGO : Shakeel, Rehan, Mehwish Sarfaraz, and Hafiz Waqas Ahmed. 2025. "Climate-Sensitive Diseases: Public Health Preparedness in the Face of Environmental Change." Global Social Sciences Review, X (II): 264-279 doi: 10.31703/gssr.2025(X-II).21
-
HARVARD : SHAKEEL, R., SARFARAZ, M. & AHMED, H. W. 2025. Climate-Sensitive Diseases: Public Health Preparedness in the Face of Environmental Change. Global Social Sciences Review, X, 264-279.
-
MHRA : Shakeel, Rehan, Mehwish Sarfaraz, and Hafiz Waqas Ahmed. 2025. "Climate-Sensitive Diseases: Public Health Preparedness in the Face of Environmental Change." Global Social Sciences Review, X: 264-279
-
MLA : Shakeel, Rehan, Mehwish Sarfaraz, and Hafiz Waqas Ahmed. "Climate-Sensitive Diseases: Public Health Preparedness in the Face of Environmental Change." Global Social Sciences Review, X.II (2025): 264-279 Print.
-
OXFORD : Shakeel, Rehan, Sarfaraz, Mehwish, and Ahmed, Hafiz Waqas (2025), "Climate-Sensitive Diseases: Public Health Preparedness in the Face of Environmental Change", Global Social Sciences Review, X (II), 264-279
-
TURABIAN : Shakeel, Rehan, Mehwish Sarfaraz, and Hafiz Waqas Ahmed. "Climate-Sensitive Diseases: Public Health Preparedness in the Face of Environmental Change." Global Social Sciences Review X, no. II (2025): 264-279. https://doi.org/10.31703/gssr.2025(X-II).21
